How to Prevent More Pandemics? Focus on the Relationship Between Humans, Wildlife, and Viruses

Patricio V Marquez
The COVID-19 pandemic is a stark reminder of the ongoing and future challenge of newly emerging infectious diseases--those that have never been recognized before, and those diseases that have been around for decades or centuries and are reemerging or resurging in a different form or location (Fauci, A 2006)
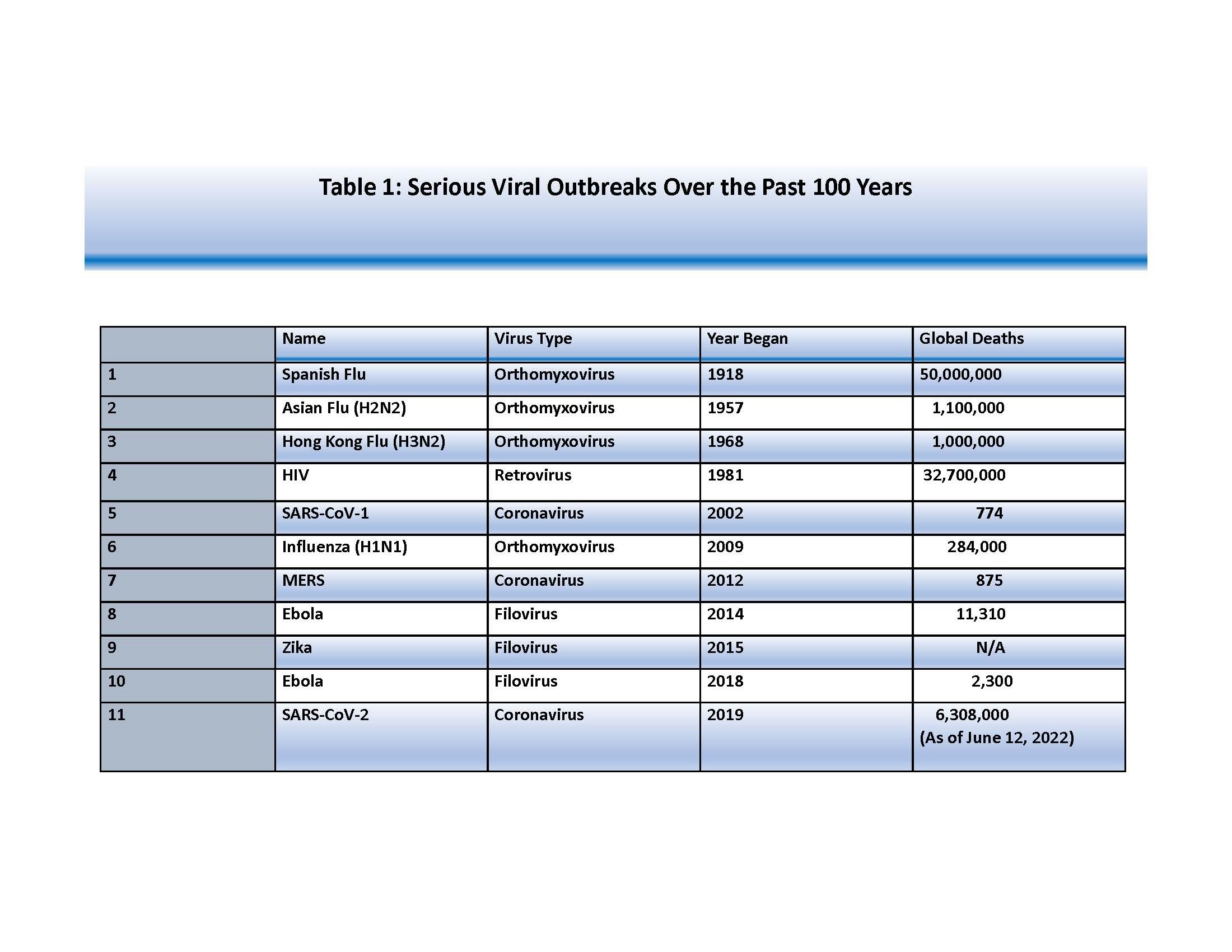
As shown in Table 1, serious viral outbreaks have occurred periodically since the early 1900s, caused by pandemic pathogens which span five virus families (US Government, 2021). Two of these outbreaks have caused more deaths than those reported from COVID-19: the Spanish Flu, which appeared in two deadly waves in 1918 and 1919, and the HIV pandemic, which has been around for more than 40 years. In addition, many other new viruses have emerged in recent decades, including the severe acute respiratory syndrome (SARS), Avian Influenza in humans, Ebola, Marburg hemorrhagic fever, Nipah virus (NiV), and the current COVID-19 pandemic, which have triggered major international concern, raised new scientific challenges, caused major human suffering and deaths, and imposed enormous economic damage. In the case of the COVID-19 pandemic, its full impact has been much greater than what is indicated by reported deaths. While the cumulative number of confirmed deaths since the beginning of the pandemic stands at 6.2 million (Our World in Data 2022), a recent paper estimates that 18.2 million people died worldwide because of the pandemic, as measured by excess mortality over that period (The Lancet 2022). Excess mortality refers to the number of deaths from all causes during a crisis above and beyond ‘normal’ conditions.
Adding to these public health challenges, yellow fever and epidemic meningococcal diseases have made a comeback in the last quarter of the 20th Century, while antimicrobial resistance (AMR), which is resistant to drugs to treat infections caused by microbes (e.g., TB), parasites (e.g., malaria), viruses (e.g., HIV) and fungi (e.g., Candida), is looming as another public health risk that has the potential to wreak similar havoc in a globalized world.
Source: Adapted from US Government, 2021; data for SARS-CoV-2 are from Our World in Data, 2022
The Crux of the Problem: Animal-Human-Environment Interface
The rising number of zoonotic diseases, diseases that are communicable between animals and humans, reflects a rise in the extent and depth of our encroachment on nature. Increasing interactions between humans and animals, the erosion of biodiversity, alteration of ecosystems, rapid urbanization and the conglomeration of people living in large mega-cities with limited access to basic services, and climate change are increasingly driving the emergence of infectious diseases, most of them from animals, and sometimes with the potential to become pandemics. Over 70 percent of emerging infectious diseases (Taylor, LH, Latham, SM, Woolhouse, MEJ 2001) have their sources in animals, domestic or wild. The transmission paths take advantage of human activities such as agriculture, logging, and mining and extraction industries that put animals and humans in closer contact than ever before (World Bank Group 2022, Berthe, F 2020, ).
Meanwhile, the over-reliance on antimicrobials to prevent and combat infectious diseases, protect plants, preserve food, and promote animal growth is giving rise to anti-microbial resistance (AMR), causing ‘superbugs’ that withstand the drugs designed to kill or inactivate them or slow their growth. Agriculture and food play a major role in the emergence and spread of diseases and AMR, due to the way food is produced, traded, and consumed (Jonas, OB, Irwin, A, Berthe, FC, Le Gall, F, Marquez, PV 2017).
How to Deal with these Recurrent Risk Factors for Human Disease Emergence?
Since these public health crises are not something new, the question that we need to ask is what have countries learned to anticipate and be ready to deal with these threats?
Earlier pandemics had provided the global community with clear warnings about the danger of fast-moving zoonotic diseases—those transferred from animals to humans, which have increased in frequency and severity, causing significant health, social, and economic damage. Each time such a disease struck, resources were hastily poured into fighting the outbreak, and calls were made to build back better, so that communities and countries would be better equipped to detect and deter subsequent crises (Horton, R 2020). Unfortunately, in many instances, it seems that once the sense of fear has diminished and the outbreak controlled, it is back to the common practice of undervaluing the importance of having in place resilient health systems anchored in robust, integrated, public health and primary care systems.
Dealing effectively with these crises requires the capacity to conduct constant disease surveillance, prompt diagnosis and case confirmation, and robust research to understand the basic biology of new organisms and our susceptibilities to them, as well as to develop effective and safe countermeasures to control them (Fauci 2006).
Detecting Risks Factors Early and Systematically
Disease surveillance is a critical public health function, but as COVID-19 has made clear, the world woefully underinvests in this function (Gates, B 2022). It is the continuous, systematic collection, analysis, and interpretation of health-related data that serves as an early warning system for impending outbreaks that could become public health emergencies. Such systems support prompt diagnosis and robust research to understand the basic biology of new organisms and our susceptibilities to them, as well as to develop effective countermeasures to control them (US CDC 2018). These systems also enable monitoring and evaluation of the impact of an intervention, help track progress towards specified goals; and monitor and clarify the epidemiology of health problems, guiding priority-setting and planning and evaluation of public health policy and strategies. An “always-on” early warning system is essential to detect disease outbreaks quickly before they spread, cost lives, and become difficult to control.
As humans have extensive contact with the environment and wildlife known to harbor vast numbers of viruses, many of which have not yet spilled into humans, better surveillance of pathogen spillover and development of global databases of viral genomics and serology, along with better management of wildlife trade, animal health management, and substantial reduction of deforestation, are vital to prevent and minimize the impact of future epidemics and pandemics.
Veterinary services have a key role to play in addressing pandemic risks at the source. By improving animal health and welfare, they fulfill the fundamental mission of protecting human populations from animal diseases, and vice-versa. This responsibility is increasingly shared by the broader community because emerging diseases are, to a large extent, driven by numerous factors, such as climate change, land use, agricultural expansion, food systems, urbanization, conflicts and war, and population mobility in an ever more interconnected world (Van Nieuwkoop, M, Eloit, M, 2021).
Country experiences show that a coordinated effort involving public health, veterinary, environmental, and social protection services, is needed to identify the strengths and weaknesses in veterinary and public health systems, develop interventions to sustain good practices, and bridge gaps to tackle the animal and human health dimensions of infectious diseases (World Bank Group 2012).
Besides passive and active public health surveillance methods, as demonstrated during the COVID-19 pandemic, strengthening public health surveillance through wastewater testing is another essential investment for anticipating and dealing with future health threats (Manuel, DG, Amadei, CA, Campbell, JR, Brault, JM, Zierler, A, Veillard, J. 2022).
In all cases, reporting systems with standard procedures and definitions are required to ensure that no cases are missed (Fauci, A 2006). Moreover, every case during an epidemic need to be regarded as a public health emergency and investigated immediately, since its chain of transmission can be used to determine the extent of virus circulation in the community. Increased laboratory capacity helps with case confirmation. Gaps in the logistics required for collecting specimens and transporting them from the field to the laboratory need addressing. Once established, laboratory support networks can help quickly analyze stool samples, and reference laboratories can provide more sophisticated tests, including genetic characterization of virus isolates.
In any type of disease outbreak, information and communication strategies are needed to help governments and regional and global institutions deliver timely notification of any outbreaks so that travelers’ advisories can be issued and response plans implemented.
All of these activities require a strong, well trained, and motivated cadre of health workers to be able to detect, identify, confirm, and inform about new pathogens and people’s susceptibilities to them, as well as to develop effective and safe countermeasures to control them.
It should be also clear, as advised by Brian Bremner in a recent book “Man Versus Microbe”, that preventing more pandemics in the future will hinge on developing a better understanding the billions of tiny pathogens circulating in nature. As he noted, if we are going to successfully handle future viral and bacterial outbreaks, we will need to head off pathogens quietly circulating in nature or within wildlife and livestock animal carriers well before they escape into human populations. That requires sustained, long-term investment in bio surveillance systems that track microbial risks at something approaching the molecular level.
These systems serve not only to monitor and interpret data of biological, chemical, and agricultural threats (Michael, M, Wagner, MM, Moore, AW, Aryel, RM. 2006), but also can help inform prevention measures and develop better-performing treatments. Innovative initiatives such as the one established between XpresSpa, Ginkgo Bioworks, and the CDC at airports in the Unites States to hunt for COVID variants by testing international travelers are a good example of real-time surveillance to monitor different biological threats in the future.
Recent technological developments are proving to be transformative, further enhancing bio surveillance and response capacity. For example, as highlighted by Bremner (2022), artificial intelligence (AI) modeled on the neural networks in human brains led to the discovery of a structurally unique antibiotic effective against dangerous strains of the bacterium Escherichia coli and drug-resistant tuberculosis. Also, as he also noted, bioengineering is disrupting animal disease vectors (e.g., genetically modified mosquitoes have been released into the air to suppress the population of an invasive species of mosquito Aedes aegypti, which transmits Zika and dengue fever and is rapidly spreading worldwide as the climate warms). Moreover, as Bremner observed, the one-year turnaround of COVID messenger RNA (mRNA) and viral vector vaccines by companies such as Pfizer, BioNTech, Moderna, and AstraZeneca--a stunning achievement in public health history--has showed that better intelligence on microbes is also key for vaccine development. Indeed, accumulated knowledge about coronaviruses from earlier epidemics of SARS and MERS contributed to this development.
‘Do no harm’: The Role of Pharmacovigilance in Implementing Countermeasures
Building capacity in countries and at the regional level to conduct thorough pharmacovigilance--the surveillance of the use of all medicines and vaccines, with particular attention to newly authorized drugs--is another critical ‘public good’ investment to ensure that the drugs work correctly and that their health benefits outweigh their known risks, serving as effective countermeasures during public health crises (Wang, H, Figueras, A, Marquez, PV, 2021; Wang, H, Marquez, PV, Figueras, A. 2022). The reporting of adverse effects and reactions after the use of a drug is a critical tool to: (i) inform decision making in a health system; (ii) educate and provide guidance to health providers; (iii) help address public safety concerns about new medicines and vaccines; and (iv) stimulate prompt policy and regulatory actions. The overall goal in undertaking this work is to improve patient care and safety with the use of any kind of medication, improve public health and safety in relation to medication use, contribute to the assessment of benefits, harm, effectiveness, and risks of medicines, and encourage safe, rational, more effective and cost-effective use of drugs in countries (WHO 2022).
The integration of pharmacovigilance with clinical practice and its further development and strengthening are vital tasks going forward to contribute to building resilience in health systems. This is of particular importance as a decades-long release of antibiotics, antivirals, antifungals, and antiparasitics into the biosphere has triggered biochemical adaptations that make infections harder to treat. Pharmacovigilance data can serve, for example, as a trigger to identify antimicrobial resistance (Habarugira, J.M.V, Härmark, L, Figueras, A. 2021). The overuse, underuse, and inappropriate use of antibiotics all contribute to the increase of AMR, which is associated with a number of clinical complications, unnecessary prolongation of hospital stays and, in some cases, death of the patient. AMR poses high costs for health systems and will be increasing in the coming years if not effectively addressed.
Moving Forward
As suggested in a new open-access book "Improving Health Care in Low-and Middle-Income Countries", improvement requires “a directed effort to take what we know can improve health – proven, high-impact interventions…. – and ensure that those are implemented reliably, in different contexts, every time…...” (Rice Marquez, L, ed. 2020).
As we emerge from the COVID-19 pandemic, it is imperative that new policy initiatives and investments in building public health preparedness and response capacity and capability rest on the recognition that preventing future pandemics means redefining the relationship between humans, wildlife, and the viruses that pass among us (Horton, R 2022). As public health and animal health are interdependent and bound to the health of the ecosystems in which they exist, it is time to accept once and for all that “One Health” (or “Planetary Health”) is not only an elegant theoretical construct, but a powerful approach to manage zoonotic risk, that can help shift the focus from a purely response mode to pre-emptive prevention and risk reduction action (World Bank Group 2010). Siloed, health sector-centric approaches will no longer suffice!
Source of Images:
Image 1: Stock Photo ID: 1975037507--A tick is sitting on the finger of man in forest on hiking path. Photo Contributor: MakroBetz.
Image 2: Stock Photo ID: 2037230357 -- Roadway video surveillance during COVID-19 on small mountain forest road between Sweden and Norway - state border closure. Photo Contributor: AlexDreamliner.