A Perspective on the AstraZeneca COVID-19 Vaccine Uncertainty
Patricio V Marquez and Albert Figueras*
As a growing number of European countries, including France, Germany and Italy, have suspended vaccination with the AstraZeneca’s Covid-19 shot temporarily, while anxiously waiting for the European Medicines Agency (EMA) and the World Health Organization (WHO) to clear up concerns over the safety of this Covid-19 vaccine, a perspective on this situation is warranted.
Let's be clear. The reality of isolated cases of blood clotting disturbances, some with unusual features such as low numbers of platelets, in recipients of COVID-19 Vaccine AstraZeneca cannot be discounted. Governments are adopting these “precautionary" measures "to be safe rather than sorry", but neither can it be ruled out that these same alterations may occur among people who have not received any vaccine recently.
When assessing events that occur after the exposure to any vaccine, the crucial point consists of establishing a relationship between the suspected cause (the vaccine in this case) and the consequence (for example, the pulmonary embolism). This is the task for physician who know the patient, the teams analyzing the reports received by the pharmacovigilance system, and the clinicians and pharmacologists working in groups such as the Pharmacovigilance Risk Assessment Committee (PRAC) of the European Medicines Agency (EMA). Until now, EMA maintains that, with the available evidence, the benefits of the AstraZeneca vaccine in preventing COVID-19, with its associated risk of hospitalization and death, outweigh the risks of side effects.
However, these events have raised alarm in countries because governments, as in other spheres of public policy, have to consider not only the evidence on the safety and effectiveness of vaccines once they began to be administered to the general population, but also the impact of potential adverse effects that are reported during a vaccination campaign on an already vaccine-hesitant population. If not handled well, these events could further undermine public confidence in COVID-19 vaccines and in government action in general, since in a large number of countries, governments are simply not trusted by the population in the handling of these concerns.
So where do these considerations leave us?
Once again, the reporting of these types of adverse effects (note that there is no evidence thus far of a cause-and-effect relationship between any COVID-19 vaccine and the reported clinical events in some people who were vaccinated), highlights the importance of pharmacovigilance as a critical tool to inform decision making in a health system. This is because before a new medicinal product such as a vaccine is marketed, its safety and efficacy exposure are limited to its use in clinical trials. Generally, clinical trials cover limited number of patients with strict inclusion criteria, often excluding special patient groups like those with co-morbid conditions, children, elderly, and pregnant women. Hence, clinical trials cannot reflect the experience in larger populations and in different geographical regions which may differ from one another with respect to genetics, food habits, life style, or clinical practices. This makes it obligatory to conduct thorough surveillance of the use of all newly authorized medical products. The review of thromboembolic events with COVID-19 Vaccine AstraZeneca is now being carried out in the context of a safety signal, which is information on a new or incompletely documented adverse event that is potentially caused by a medicine such as a vaccine and that warrants further investigation under an accelerated timetable.
There are many factors that have converged to lead to the current situation with the Oxford/AstraZeneca Covid-19 vaccine, as it happened with the first cases of anaphylactic reactions reported in people after receiving an mRNA vaccine some weeks ago. They can be summarized as follows:
- Recent products were developed in record time and are now massively used. Typically, the development of new vaccines requires years of research and testing before being deployed. In the case of the new COVID-19 vaccines, scientists have been racing to produce a safe and effective vaccine in record time. In a historical feat, the trials of some of the vaccines have taken less than a year. And beginning in early December 2020, COVID-19 vaccines are the first example in history in which millions of people have used a new medicine/product across the world in just three months. Indeed, more than 381.34 million vaccine doses have been administered worldwide as of today, equal to 4.7 doses for every 100 people; the total number of people who have been fully vaccinated against COVID-19 using different vaccines amounts to 86 million people or about 1.1% of the total population in the world.
- The need to act quickly because stopping or reducing vaccination speed for one week could mean thousands of newly infected people (and potentially hundreds of preventable deaths), particularly in the European Union countries, that are facing a new wave of COVID-19 infections. On the other hand, as investigating reported side-effects and severe events is vital in a vaccination campaign, dismissing an adverse effect truly related to the vaccine could also mean increased morbidity and mortality.
- Political consequences of a too-early or a too-late decision. Although counterintuitive, it is not easy to make decisions at the country level just by following scientific advice. The present pandemic has shown this in different moments in the last 12 months. The scientific reasoning is not well understood, and there are many players behind any political decision.
- Lack of real knowledge. To assess an adverse event after receiving a vaccine or medicine, it is necessary to know many clinical details (not always available), patient comorbidities, and other concomitant medications. After reviewing all these data, it is possible to strengthen the suspicion or to discard it. Thus, each report requires an additional detailed investigation before concluding. Also, one of the crucial points to consider is the occurrence of a disease such as the reported one due to other causes. This explains why the PRAC statement says: "the incidence of thromboembolic events in the vaccinated population is no greater than the incidence in the general population".
Within this context, there is a final consideration (which perhaps should be the first one): how to manage the lack of precise data in the era of information (and misinformation), social media, quick spreading of news, and leaked information. All this merits further discussion and, yes, vigilance, as the "do no harm" principle should be the guiding rod to follow in vaccination campaigns, particularly to preserve public trust in countries with high vaccine hesitancy like France, that if eroded, could negatively impact on the public take-up of COVID-19 vaccines.
So, in conclusion, with the information available today in the midst of a killer pandemic of historical repercussions affecting all walks of life, we, as individuals, will take any of the COVID-19 vaccines authorized by regulatory authorities without any doubt or concern. However, the point that matters most and that requires utmost attention and careful navigation is how we communicate clearly to vaccine-hesitant populations who do not trust governments in the first place, information that is anchored in good-quality data on vaccine safety and side effects. That is at the crux of this current situation, and it cannot simply be disregarded, because it could occur with any of the other COVID-19 vaccines that have received emergency use authorization by either a stringent regulatory authority such as the US Food and Drug Administration (FDA) and the EMA, or by WHO.
On this matter, we will do well to remember the wise words of Henry Sigerist, the early 20th Century director of the Johns Hopkins University Institute of History of Medicine, who observed that: "It is quite obvious that the means and methods used in the prevention of disease are those provided by medicine and science. And yet, whether these methods are applied or not, does not depend on medicine alone, but to a much higher extent on the philosophical and social tendencies of the time."
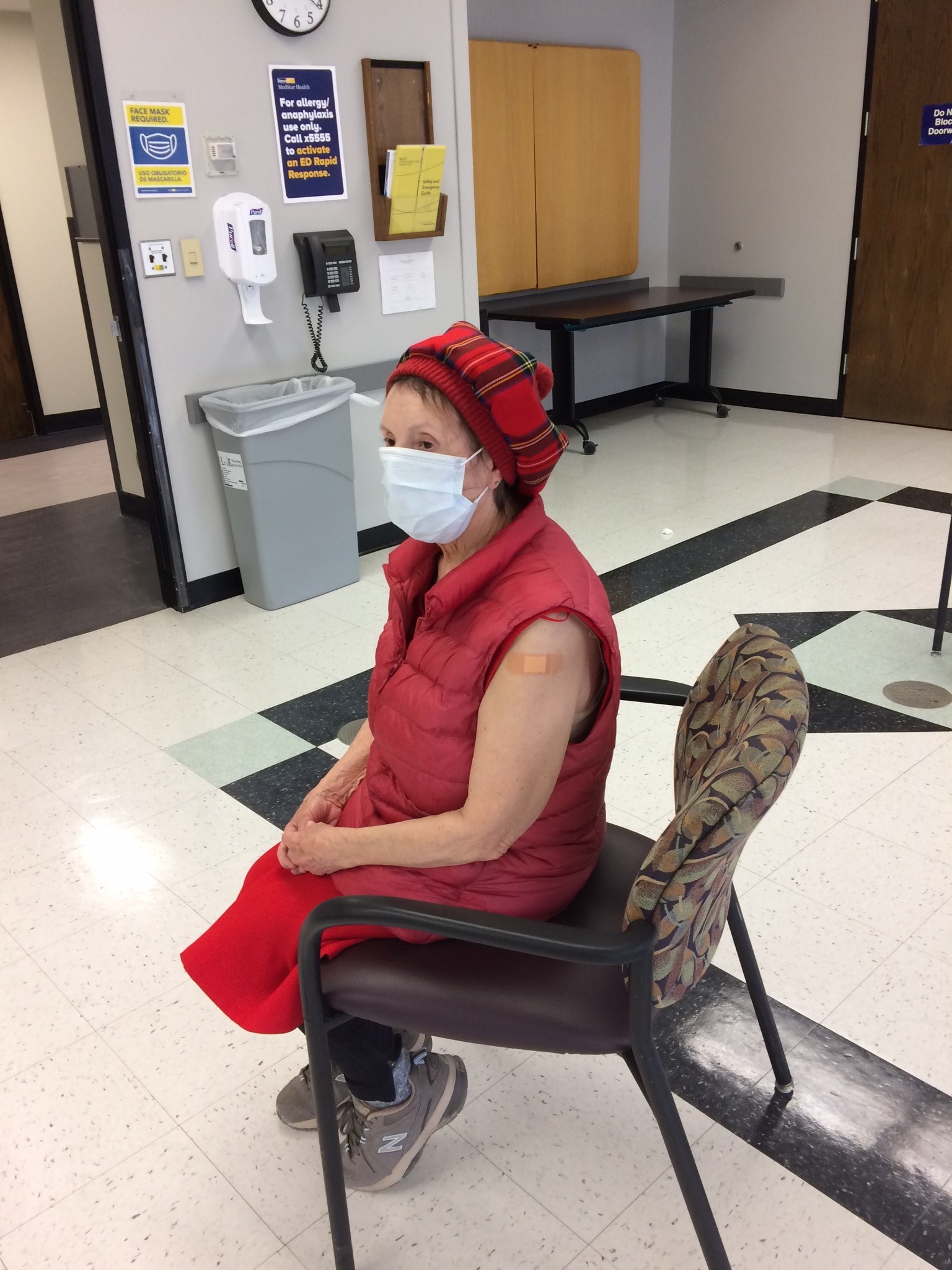
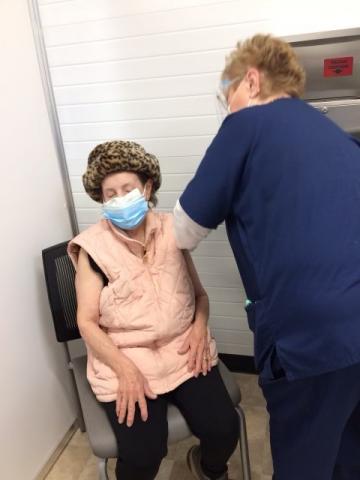
Picture: The 87-year old Mother of one of the authors, Sra. Elena Marquez, being administered the COVID-19 vaccine.
*Former Director of the Catalan Institute of Pharmacology (Fundació Institut Català de Farmacologia, FICF), which is associated with the Department of Pharmacology, Therapeutics and Toxicology at the Autonomous University of Barcelona (UAB) and serves as a WHO Collaborating Center for Research and Training in Pharmacoepidemiology.