On World Health Day 2024: Let’s Remember that Most Deadly Behavioral Risk Factors Are Preventable

Patricio V Marquez
April 7, 2024
“The devastation that Covid-19 has inflicted globally is truly historic and highlights the world’s overall lack of public health preparedness for an outbreak of this magnitude.”
Anthony S. Fauci
“It Ain’t Over Till It’s Over…but It’s Never Over — Emerging and Reemerging Infectious Diseases”,
N Engl J Med 2022
This year, on April 7th, World Health Day 2024 is observed under the theme 'My Health, My Right’. The theme was chosen by the World Health Organization to champion the right of everyone, everywhere to have access to quality health services, education, and information, as well as safe drinking water, clean air, good nutrition, quality housing, decent working and environmental conditions, and freedom from discrimination.
While the loftiness and ambitiousness of the theme deserve to be supported as the end objectives of the global development agenda over the medium term, around the world the right to health of millions is under threat by risk factors that can be prevented by decisive and sustained implementation of policy measures known to be effective.
Risk Factors Burden
As highlighted in the 2019 Global Burden of Disease (GBD) study, highly preventable risk factors, which are contributing to the growing burden of non-communicable diseases (NCDs) and injuries, are rising at alarming rates, adding to the perpetual health and societal challenge posed by emerging and re-emerging infectious diseases. GBD data show that NCDs are already a dominant burden of disease, accounting for three quarters of global deaths. And, as the COVID-19 pandemic made evident, the intersection between infectious diseases and NCDs requires focused attention and action targeting the broader determinants of health upstream. Such measures are essential to manage the significant burdens these diseases impose on global health, social, and economic systems.
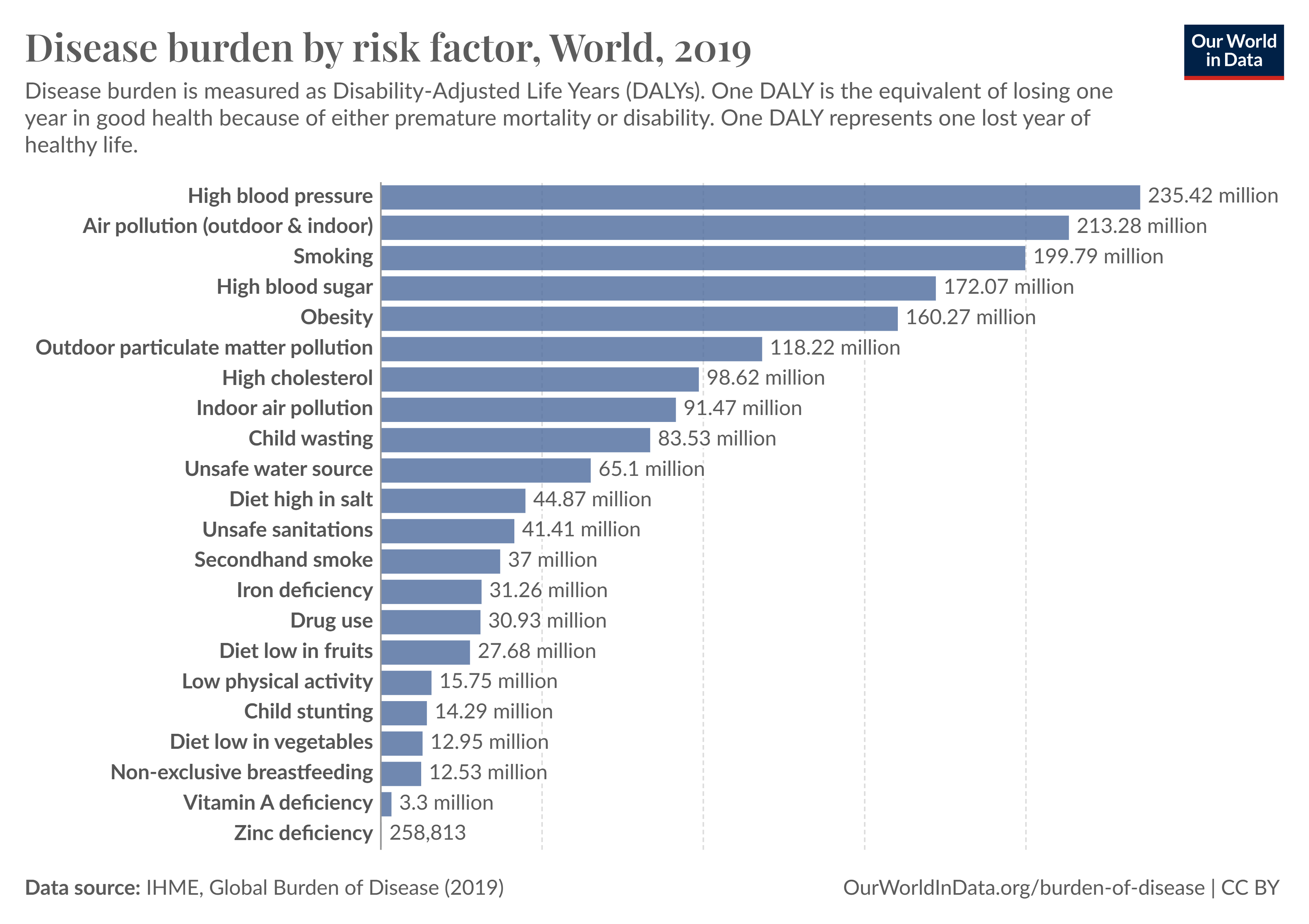
The GBD study framework classified risks in three major risk factor groups: a) metabolic, b) behavioral, and c) environmental and occupational. Figure 1 shows the disease burden by risk factor. The GBD 2019 study estimated that around 48 percent of the overall disease burden in 2019, measured in disability-adjusted life years (DALYs), can be attributed to these risk factors. With about 831 million DALYs, the behavioral risk factors account for the highest attributable burden, followed by 463 and 397 million DALYs for metabolic and the group of environmental and occupational risks, respectively. Reducing exposure to these risk factors would have significant health and societal benefits, helping to realize the 'My Health, My Right’ global aspiration.
Figure 1:
Commercial Determinants of Health
Commercial determinants of health refer to the influence of private sector activities on public health, which can be either beneficial or detrimental. These activities encompass various aspects such as the provision of products and services for profit, marketing strategies, working conditions, production effects on health, and political engagement, including lobbying and misinformation campaigns.
The 2019 Global Burden of Disease study revealed that diseases that stand as leading causes of death and disability worldwide are significantly driven by behavioral risk factors associated with the consumption of legally traded commercial products. The consumption of specific unhealthy products permeates all levels of society, demonstrating a pervasive influence across demographic groups and geographical regions. Among these, tobacco use, alcohol abuse, and the consumption of unhealthy foods—particularly sugar-sweetened beverages—stand out.
Tobacco use, whether through smoking, chewing, or vaping, remains one of the most detrimental addictions to human health. The harmful chemicals present in tobacco products harm nearly every organ of the body, predisposing individuals to a wide array of chronic conditions. From respiratory ailments like chronic obstructive pulmonary disease (COPD) to several cancers, heart disease, stroke, diabetes, and other chronic health conditions, tobacco use significantly heightens the risk of morbidity and mortality. The impact also extends beyond the person who smokes putting others at risk of developing tobacco-attributable diseases (for example, smoking during pregnancy not only increases the risk for pregnancy complications, but tobacco smoke harms babies before and after they are born). Globally in 2019, tobacco use was responsible for 8.7 million deaths or 15.4 percent all deaths, and 7.9 percent of healthy life lost (DALYs).
Similarly, the harmful use of alcohol poses a significant threat to long-term health. While moderate alcohol intake may have certain benefits, such as the potential protective effect on cardiovascular health, excessive and chronic alcohol consumption can lead to several serious health conditions, including cirrhosis of the liver, fetal alcohol syndrome, chronic illnesses such as heart disease, stroke, and some cancers, interpersonal violence, self-harm (suicide), drunk driving–related injuries, and other unintentional injuries. Furthermore, alcohol consumption often contributes to the development of comorbidities, exacerbating existing health conditions and diminishing overall well-being. In 1990, alcohol use was the 13th most relevant risk factor for deaths worldwide; in 2019, it has risen to the 8th most relevant risk factor, responsible for over 2.4 million deaths from various alcohol-attributable causes, and 3.7 percent of DALYs. In 2019, alcohol use was the leading risk factor among males aged 15–49 years, and young people tend to experience a higher rate of injuries as a result of alcohol use, leading to an increase in death and disability for that age group.
The widespread consumption of unhealthy foods, particularly those containing added sugars such as sugar-sweetened beverages, is a growing global concern. Marketed as refreshing and enjoyable, these beverages are high in calories but offer little nutritional value. Regular consumption can lead to weight gain and obesity, which in turn increases the risk of various chronic diseases including type 2 diabetes, cardiovascular diseases, certain cancers, and musculoskeletal disorders. Moreover, the excessive intake of sugary beverages can contribute to insulin resistance, establishing a significant connection between their consumption and the development of type 2 diabetes. Research spanning diverse populations indicates a steady increase in obesity rates from less than 1 percent to 6–8 percent among children, from 3 percent to 11 percent among men, and from 6 percent to 15 percent among women between 1975 and 2016. Obesity now affects over 2.1 billion individuals or nearly 30 percent of the global population.
A Way Forward
Looking ahead, it is imperative to acknowledge that countries, regardless of their economic status, cannot afford to wait to ‘treat their way out” of disease and disability. While universal health coverage remains a critical global goal for ensuring accessible and affordable medical care, it is essential to strike a better balance by placing added emphasis on health promotion, disease prevention, and pandemic preparedness.
The underlying health risk factors and their syndemic or interconnected nature fueling the rise in chronic conditions and injuries are not only widely recognized and documented but also largely preventable targeting both the whole population and high-risk groups. Tackling these factors upstream demands first and foremost decisive action to deal with political inertia, social inequality, disinformation, and a lack of preparedness, in addition to concerted multi-sectoral strategies and societal changes to foster healthier lifestyles and alleviate the burden of chronic diseases and comorbidites on individuals and societies alike.
We can draw valuable lessons from recent public health successes, such as the consistent decline in global smoking prevalence since 1990, by 27.5 percent among men and by 37.7 percent among women. These successes underscore the pivotal role of government intervention through tax laws and regulations, increased health literacy, as well as the implementation of other demand and supply measures outlined in the Framework Convention on Tobacco Control, the first international health treaty negotiated to deal with the globalization of the tobacco epidemic.
However, despite the knowledge gained from accumulated global experience, many countries still lag far behind in enacting necessary legislation and implementing sustainable actions to address public health issues effectively. As we observe World Health Day 2024, let us hope that governments worldwide will reassess social priorities and renew their commitment to support sustained action to ensure that the right to health becomes a concrete reality for millions globally, rather than just a lofty rhetorical aspiration.
Source of Image:
World Health Organization WHD2024 - campaign material
